There are two types of neurological patients – 1) those who come in with clearly defined neurological symptoms and/or signs (headache, diplopia, APD, disc edema, constricted confrontations, etc) and 2) those who come in with vague visual symptoms and no clear pathology on dilated exam. The first type of neurological patient is often easy to recognize but the second type of neurological patient often requires more time and investigation. Besides vision, pupils, and motility, visual field testing is one of the most important tests you can obtain for these identifiable (or often unidentifiable) neurological patients. Visual field testing not only localizes the problem, the defect pattern can narrow your diagnosis and allow you to be more precise in your management/referral. Most, if not all, of these patients will require urgent neuroimaging and multidisciplinary care. Most, if not all, of these patients will be anxious and scared of the unknown while you investigate the root cause of their neurological visual field defect. The more comfortable you feel with neurological diagnoses and how they present, the more comfortable the patient will feel as they navigate the next step in their treatment.
The neurological patient: symptoms
Occasionally, patients will present with a neurological visual field defect and deny any and all neurological symptoms. More often than not, patients will present with one or more of the following neurological symptoms:
- Headache, typically daily
- Change in vision
- Double vision
- Numbness/weakness of one side of the body
- Confusion
- Fatigue
- Change in mood
- Stiff neck
- Nausea/vomiting
- Difficulty speaking or comprehending
Keep in mind that patients may not voluntarily divulge this information because they don’t see a connection between their recent change in mood and their eyes. Often times the provider will need to ask specific questions to elicit some of these symptoms that these patients may be dealing with on a day to day basis.
The neurological patient: signs
From patient demographics to health history to family history to the clinical exam itself, every aspect provides insight into the patient’s diagnosis. Some patients may present with a clean health history and an unremarkable eye exam (other than the visual field, of course). Other patients may present with a list of cardiovascular conditions, have elevated blood pressure in office, and show retinal-vascular changes on posterior segment evaluation. Other patients may present with decreased vision, pain on eye movement, and a swollen (or non-swollen) optic nerve. The clinical exam will vary but it is important to be aware of various neurological conditions, including what populations they are often found in and how they may present on exam.
The neurological visual field: various defects
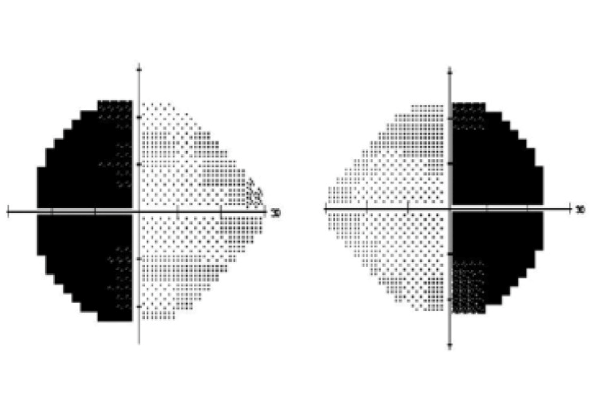
1. Heteronymous hemianopsia (bitemporal hemianopsia)
The most common heteronymous hemianopsia is the bitemporal hemianopsia. This visual field defect is characterized by vision loss respecting the vertical midline and affecting the opposite side of vision in both eyes (or the temporal vision of each eye). This visual field defect is mostly common caused by a pituitary adenoma, but can also be caused by a craniopharyngioma &/or a suprasellar aneurysm or meningioma.
2. Homonymous quadranopsia/hemianopsia
This visual field defect is characterized by vision loss respecting the vertical midline and affecting the same side of vision in both eyes. The visual field loss will affect the vision to the side opposite the lesion. For example, a stroke to the right occipital lobe will create a left-sided hemianopsia. This type of visual field defect can be caused by stroke &/or mass affecting various aspects of the brain. Visual field patterns can often help localize the neurological lesion. Lesions affecting the optic tract (more anterior in the visual pathway) will create a more incongruous/asymmetric hemianopsia. Lesions affecting the occipital lobe (more posterior in the visual pathway) will create a more congruous hemianopsia. Lesions affecting the optic radiations of the parietal lobe will create an inferior quadranopsia and lesions affecting the optic radiations of the temporal lobe will create a more superior quadranopsia.

3. Other
Neurological lesions may not be cookie-cutter clean. They may affect multiple areas of the visual pathway, causing variations of the classic visual field defects we know and expect. They may cause diffuse visual field loss or more localized loss in the form of central scotoma, centrocecal scotoma, altitudinal defect, and/or arcuate-like defects. This varying degree of visual field loss is often found in patients with optic neuritis. Although optic neuritis is a pre-chiasmal condition, its significance lies in its connection to demyelinating disorders of the central nervous system, such as multiple sclerosis or neuromyelitis optica.
The neurological patient: management
So you’ve identified that your patient has a neurological visual field defect with associated neurological symptoms. Now what?
Order the imaging. Most of these cases require urgent or emergent imaging. Narrowing down a diagnosis or likely etiology will help you determine what neuroimaging to order.
- Computed tomography (CT). With respect to neurological visual field defects, the CT scan is most beneficial at identifying/locating a suspected tumor &/or identifying/locating a stroke or hemorrhage. Depending on the urgency of imaging, CT scans can often be obtained faster (especially in ER settings) and are often less expensive. Example: Order CT scan of head with and without contrast to rule out XYZ.
- Magnetic Resonance Imaging (MRI). With respect to neurological visual field defects, the MRI is typically preferred due to improved detail of soft tissue. The MRI can identify MS lesions in white matter, identify/locate various masses/tumors (especially pituitary tumors), and identify/locate ischemic damage and/or aneurysm. MRI scans typically need to be pre-authorized and are more costly. Keep in mind that an MRI is contraindicated in patients with pacemakers, defibrillators, or other implanted electronic devices; previous neurosurgical clip placement; metallic foreign bodies; insulin pumps; and claustrophobia. Example: Order MRI of brain and sellar region
 with multiplanar thin sections with and without contrast to rule out brain lesion causing optic chiasm compression.
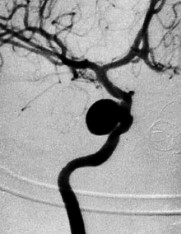
with multiplanar thin sections with and without contrast to rule out brain lesion causing optic chiasm compression. - CT or MR angiography (CTA/MRA). With respect to neurological visual field defects, the CTA/MRA should be ordered in addition to the CT or MRI scan if there is any concern for aneurysm. These scans examine blood vessels and blood flow to identify aneurysms, blood clots, vessel stenosis, and/or abnormal vasculature feeding a tumor.
When the imaging results come back, you have two primary tasks. First and foremost, contact the patient (preferably in office vs. over the phone) and discuss the test findings. It’s important to allow the patient to digest the news and be prepared for their questions regarding the next steps. It’s equally important to be there for your patient and to offer empathy. Second and equally as important, contact the primary care provider to help with referrals to the appropriate specialties. It may be as simple as better cardiovascular control in a stroke patient. It may be more complex, such as a referral to the endocrinologist and neurologist/neurosurgeon in a patient with confirmed pituitary adenoma. In any case, your role as a primary eye care provider just helped identify the problem and jumpstart the appropriate road to recovery. Bravo. Your patient will be forever grateful.
References:
- https://www.uptodate.com/contents/optic-neuritis-pathophysiology-clinic-features-and-diagnosis#H5
- https://www.reviewofoptometry.com/article/an-intro-to-neuro
- https://www.healthline.com/health/ct-scan-vs-mri#takeaway

Author: Alana Curatola, OD
Renton Clinic
I chose the topic of neurological visual field defects because of the importance of this topic. These cases tend to be more rare and it’s crucial to recognize neurological signs and symptoms as well as be familiar with how various neurological conditions can present on visual field testing. Being comfortable with neurological visual field defects can help narrow a diagnosis and point you in the right direction as far as how to proceed. As they always say, it’s not rare until it’s in your chair. Over the past 2 years at Northwest Eye Surgeons, I have seen at least 5 patients who presented with neurological symptoms &/or a neurological visual field defect. After further imaging, these patients went on to have a diagnosis of multiple sclerosis, cerebrovascular accident, intracranial ICA aneurysm, and pituitary adenoma. Not every patient has a happy ending in these types of cases but it’s cases like these that make this career extra rewarding. The eyes are truly windows into the body and I enjoy the detective work. I enjoy working with other providers across different medical specialties to better serve our patients and their various conditions.









