Plaquenil (hydroxychloroquine) has been thrusted into the spotlight due to the current COVID-19 pandemic. Its off-label use has been used a potential therapy for the virus, all data being anecdotal at best. Before COVID-19, Plaquenil was first used as an anti-malarial, but quickly started being used for a myriad of autoimmune diseases. The anti-inflammatory effects helped these patients return to a normalcy in everyday life. In the clinic these often present as recent diagnosis of rheumatoid arthritis (RA) or Systemic Lupus Erythematosus (SLE), two autoimmune conditions that already present with ocular findings.
The mechanism of toxicity it not yet fully understood. The drug appears to bind to melanin which is located in the retinal pigmented epithelium (RPE) and over accumulates causing atrophy. The classic bull’s eye presentation occurs when melanin accumulates in the RPE parafoveally. Clinically this is seen in the late stage of drug toxicity. It is important to understand that even after drug cessation toxicities can continue to occur. Identifying the earliest maculopathies with specialized testing is crucial for preserving vision. Risk of toxicity up to 5 years is under 1% and up to 10 years is 2%. The risk increases to 20% after 20 years of use. The other risk factors that can exacerbate retinal toxicity are concomitant renal disease, retinal disease and the use of tamoxifen.
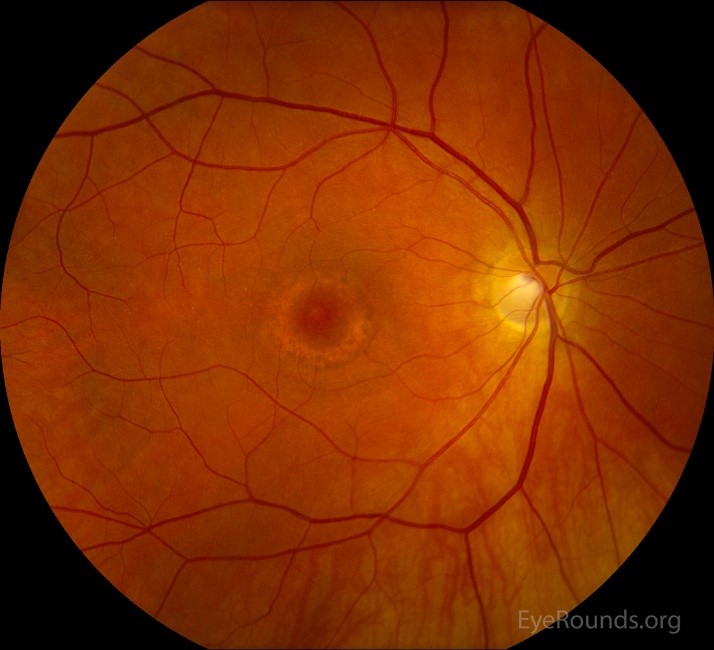
Late stage bull’s eye maculopathy. (https://webeye.ophth.uiowa.edu/eyeforum/atlas/pages/Hydroxychloroquine-toxicity/plaquenil-fundus-OD-LRG.jpg)
Clinically, we are able to catch the earliest signs of toxicities using Humphrey Visual fields and Spectral domain-OCT (SD-OCT). These two tests are relatively easy to administer and produce reliable results for clinicians to interpret.
The screening examination for Plaquenil toxicity includes evaluation of the central visual field, a 10-2 is recommended with white stimulants. In patients from Asian ancestry, a widened visual field is used because the RPE tends to be affected outside of the central ten degrees. An appropriate visual field would therefore be 24-2 or the 30-2.
SD-OCT is then utilized to visualize the health of the underlying RPE and photoreceptor integrity line (PIL). Preexisting maculopathies might exacerbate Plaquenil toxicities. Identifying a healthy RPE and PIL without abnormalities is vital to establish a reliable baseline.

OCT showing PIL loss in the parafovea. (https://cdn.ymaws.com/www.opsweb.org/resource/collection/7BB07D9E-C5D6-4FED-82FB-58D7C407D5B3/Snodgrass_Plaquenil_30_min.pdf)
Patients on high doses for long durations are at highest risk for maculopathies. The recommended maximum daily Plaquenil use is 5mg for every kilogram of real weight. This calculation should be accomplished for each patient to ensure proper recommendations for the referring provider. Once the initial screening is complete and base lines are established, annual screenings are recommended after 5 years of therapy. If the patient has concomitant renal disease, retinal disease or tamoxifen use, annual screenings should be considered before the 5-year marker.
As the population in our area rises, we are guaranteed to see a rise in our referrals from primary care and rheumatologists. Being at the forefront of our screening skills will ultimately better serve our patients. The majority of patients on long term Plaquenil therapy never develop vision loss, but to the several that do, a keen eye and specialized testing can help preserve their vision.
References:
Gbinigie, Kome, and Kerstin Frie. “Should Chloroquine and Hydroxychloroquine Be Used to Treat COVID-19? A Rapid Review.” BJGP Open, vol. 4, no. 2, 2020, doi:10.3399/bjgpopen20x101069.
Marmor, Michael F., et al. “Recommendations on Screening for Chloroquine and Hydroxychloroquine Retinopathy (2016 Revision).” Ophthalmology, vol. 123, no. 6, 2016, pp. 1386–1394., doi:10.1016/j.ophtha.2016.01.058.
Michelson, Matthew, et al. “Ocular Toxicity and Hydroxychloroquine: A Rapid Meta-Analysis.” 2020, doi:10.1101/2020.04.28.20083378.

Author: Ali Mainayar, OD
Specialties: Medical Eye Care
Renton Clinic
A patient that I followed regularly during residency had Plaquenil toxicities from being misdiagnosed with SLE and on the wrong dose for her real body weight. The toxicities all presented after the cessation of the drug. She was unfortunately left with no functional vision in either of her eyes. This case demonstrated firsthand how crucial it is to have proper screening and to monitor for early changes. My brief tenure with Northwest Eye Surgeons thus far has already yielded a handful of screening referrals. My passion in retinal disease encompasses drug toxicities. The eyes help us monitor systemic conditions, drug toxicities is something we often overlook when assessing the retina.









