While serving in the military, I had the opportunity to work with a significant number of patients diagnosed with traumatic brain injury (TBI). The effects this can have on a patient’s visual system are numerous and varied. Though TBIs are not as prevalent in civilian life, they do occur for a variety of reasons and can be life changing for patients. With popular media shedding more light on sports and TBIs in particular, including youth sports, I thought it would be a good idea to provide a refresher on optometry’s role in treating TBI patients. This blog is not intended to present an in-depth discussion of this important issue, though perhaps a future continuing education opportunity could dive deeper!
Traumatic brain injuries (TBI) are defined by the CDC (Centers for Disease Control) as “a bump, blow or jolt to the head or a penetrating head injury that disrupts the normal function of the brain.” TBIs range from mild to severe, but all levels of severity can cause temporary or ongoing effects. The CDC reports approximately 2.8 million annual TBI events in the United States with falls as the leading cause. In addition, TBI has been found to be one of the leading causes of lifetime disabilities and death in the United States, with an estimate of over 3 million people at the start of 2005 with TBI induced lifetime disabilities.
No matter the mechanism of injury, TBIs can result in a wide array of visual symptoms. Several studies have found approximately 60% of TBI patients will experience a visual difficulty or abnormality.
Common visual effects with TBI:
- Change in refraction, loss of visual acuity
- Abnormal color discrimination and contrast sensitivity
- Visual field defects
- Abnormal accommodation
- Abnormal vergence, phorias or strabismus
- Abnormal eye movements: nystagmus, pursuits, saccades or fixations
- Lagophthalmos, abnormal pupils, ptosis
- Visual perception abnormalities, neglect and visual midline shift syndrome/ abnormal egocentric localization
- Light sensitivity/photosensitivity
- Ocular structure trauma (possible with recent TBI event)
Common patient concerns after TBI:
- Blurred vision
- Difficulty with reading
- Double vision
- Light sensitivity (overhead lights, outdoors and backlit screens)
- Headaches and eyestrain
- Dry eyes
- Bumping into objects or wall, dizziness, balance issues
In addition to the above symptoms, Dr. William Padula describes what he names “Post-Traumatic Vision Syndrome.” He has categorized several symptoms under this heading, including: accommodative dysfunction, convergence insufficiency, exotropia/high exophoria, poor fixations and pursuits, lowered blink rate, unstable ambient vision, visual midline shift syndrome and spatial disorientation.
Each clinician evaluating TBI patients should have some form of clinical work-up in mind that can be easily fine-tuned based upon different patient concerns and presentations. A longer exam time is typically recommended due to other mental processing issues that may result after TBI. If not possible, consider breaking the exam into different days: for example, a full comprehensive exam one day and a binocular vision work-up with extra testing a different day. In depth questioning should also be performed for case history. Many patients don’t realize how many different symptoms an optometrist can investigate for them, such as headaches or reading problems. Examination should include a comprehensive ocular health check, refraction (with special care to prevent overminusing), binocular vision work-up, visual field screener and eye movement evaluation. Visual information processing testing and oculography for reading eye movements should also be considered based upon patient’s symptoms, if possible. Again, based upon patient concerns, monitor for midline shifts or other abnormal ambient and focal processes (example: extinction/neglect syndrome).
It seems likely that TBIs will continue to be prevalent. Health care professionals, including optometrists, should be willing and able to assist TBI patients down their road to recovery; keeping in mind that achieving pre-injury levels of function should not be the overall goal, but rather achieving the best possible post-injury potential. It is important that a multidisciplinary team approach be taken with TBI patients. Referrals should be based upon patient symptoms and often involve occupational therapy, physical therapy, neurology and psychology/psychiatry. It should be noted that entire books have been written on this subject and many studies continue to be conducted. Be willing to educate yourself and your staff members so that you may also educate patients and provide the extra steps they may need to have a healthy and happy visual system.
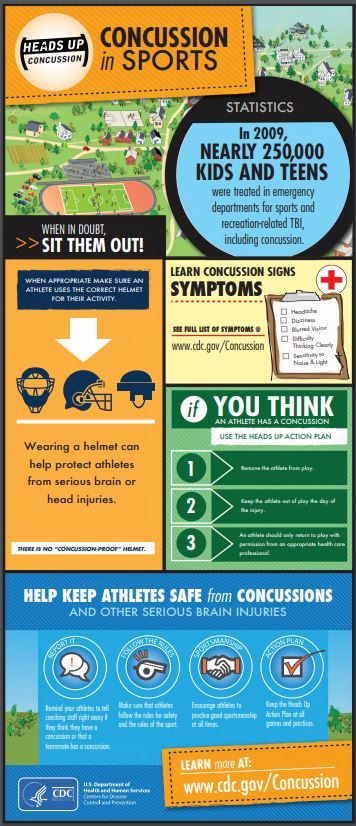
The CDC has a great “HEADS UP” program to help prevent and treat TBI in youth. There are numerous online resources, including training links, diagnostic tools and PDF visuals, as shown below in one of my images. This site provides a thorough overview: HEADS UP link
CDC Factsheet about Concussions and Brain Injury, PDF
The Neuro-Optometric Rehabilitation Association, or NORA, is a great resource for more information. One of their recent news emails shared an article published on Healio that discusses some new technology becoming available to optometrists to TBI evaluations, take a look: New technology for concussion and visual function
Below is a snapshot of resources that I have used in the past to research TBIs and vision. This blog was a means to get readers thinking about their TBI patients and guidance to strive to positively impact their visual health.
REFERENCES
- Adams, Elizabeth. Visual Problems in Traumatic Brain Injury: A Systematic Review of Sequelae and Interventions for the Veteran Population. Department of Veterans Affairs: VHA Office of Patient Care Services, Technology Assessment Program. http://www.va.gov/optometry/docs/vistbi-vision-tbi-final-report-9-09.pdf
- What is the Glasgow Coma Scale? http://www.brainline.org/content/2010/10/what-is-the-glasgow-coma-scale.html
- Cockerham, G.C., et al. Eye and Visual Function in Traumatic Brain Injury. Journal of Rehabilitation Research and Development. 2009; 46 (6): pp 811-818.
- Defense Centers of Excellence. Defense and Veterans Brain Injury Center. http://www.dcoe.mil/content/Navigation/Documents/About%20DVBIC.pdf
- Dougherty, A.L, et al. Visual Dysfunction Following Blast-Related Traumatic Brain Injury from the Battlefield. Brain Injury, January 2011; 25 (1): pp 8-13.
- Girgis, Nadine. Back to the Basics, Part 4: The Diagnosis Behind Diplopia. Review of Optometry. 2008. https://www.reviewofoptometry.com/article/back-to-the-basics-part-4-the-diagnosis-behind-diplopia
- Goodrich, G.L., et al. Mechanisms of TBI and Visual Consequences in Military and Veteran Populations. Optometry and Vision Science, Feb 2013, Vol 90, No. 2: pp 105-112.
- Gottlieb, D. Method of Using a Prism in Lens for the Treatment of Visual Field Loss. United States Patent number 4,779,972. Oct 1988.
- Hock, Daniel R. and Coffey, Bradley. Effects of Yoked Prism on Spatial Localization and Stereolocalization. Journal of Behavioral Optometry. 2000. Vol 11 (6): pp 143-148.
- Kadet, Theodore S. Neuro-Optometric Treatment for Medically Stable Patients. Neurorehabilitive Optometry guest lecture. Pacific University College of Optometry. 16 July 2012.
- Kaplan, Melvin. Seeing Through New Eyes: Changing the Lives of Children with Autism, Asperger Syndrome and Other Developmental Disabilities Through Vision Therapy. Jessica Kingsley Publishers. Philadelphia, PA and London N1 9JB, UK. 2006.
- Königs, M., et al. Impaired Visual Integration in Children with Traumatic Brain Injury: An Observational Study. PLOS One. December 2015. http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0144395
- Kraus, M.F., et al. White Matter Integrity and Cognition in Chronic Traumatic Brain Injury: A Diffusion Tensor Imaging Study. Brain, 2007; 130, pp 2508-2519.
- Kussman, Michael J. Performance of Traumatic Brain Injury Specific Ocular Health and Visual Functioning Examinations for Polytrauma Rehabilitation Center Patients. Department of Veterans Affairs, Veterans Health Administration, VHA Directive 2008-065. October 2008.
- Laukkanen, Hannu. ABI/TBI Testing. Neurorehabilitive Optometry lecture. Pacific University College of Optometry. 20 May 2012.
- Laukkanen, Hannu. ABI/TBI Treatment Overview. Neurorehabilitive Optometry lecture. Pacific University College of Optometry. 14 July 2012.
- Laukkanen, Hannu. Specific Treatments with TBI: Yoked Prisms and VT. Neurorehabilitive Optometry lecture. Pacific University College of Optometry. 14 July 2012.
- McVeigh, Francis. Traumatic Brain Injury: What is the Optometrist’s Role? Review of Optometry. April 2008. https://www.reviewofoptometry.com/article/traumatic-brain-injury-what-is-the-optometrists-role
- Padula, W.V. and Argyris, S. Post Trauma Vision Syndrome and Visual Midline Shift Syndrome. NeuroRehabilitation, 1996; 6, pp 165-171.
- Peli, Eli. Fitting Peripheral Prisms for Patients with Hemianopia. Power Point Presentation. Schepens Eye Research Institute, Massachusetts Eye and Ear. 2011. http://www.aaopt.org/sites/default/files/WK-02.pdf
- Richman, Elaine A. Traumatic Brain Injury and Visual Disorders: What Every Ophthalmologist Should Know. American Academy of Ophthalmology. March 2014. http://www.aao.org/eyenet/article/traumatic-brain-injury-visual-disorders-what-every-2
- Scheiman, Mitchell and Wick, Bruce. Clinical Management of Binocular Vision: Heterophoric, Accommodative, and Eye Movement Disorders: Third Edition. Lippincott Williams and Wilkins, a Wolters Kluwer business. Philadelphia, PA. 2008.
- Schmalzle, Joy A. The Visual Consequences of Traumatic Brain Injury Course. Online continuing education course (COPE Course ID: 37700-NO). April 2015.
- Shenton, et al. A Review of Magnetic Resonance Imaging and Diffusion Tensor Imaging Findings in Mild Traumatic Brain Injury. Brain Imaging Behavior. June 2012: 6(2): 137-192.
- Suchoff, Irwin B., e tal. Visual and Vestibular Consequences of Acquired Brain Injury. Optometric Extension Program Foundation, Inc. Santa Ana, CA 92705-5510. 2001.
- Suter, Penelope S. and Harvey, Lisa H. Vision Rehabilitation: Multidisciplinary Care of the Patient Following Brain Injury. CRC Press. Boca Raton, FL. 2011.
- Teasdale, G. et al. Forty Years On: Updating the Glasgow Coma Scale. Nursing Times, 2014; 110 (42),pp 12-16.
- S. Department of Health and Human Services: Centers for Disease Control and Prevention. Get the Stats on Traumatic Brain Injury in the United States. 2006. http://www.cdc.gov/traumaticbraininjury/pdf/BlueBook_factsheet-a.pdf
- Vaughan, Don. TBI Prognosis. Military Officer. March 2016. P 92-95; 108-110.

Author: Leigh M. Gongaware, OD, MS
Bellingham and Mount Vernon clinics
Working at Northwest Eye Surgeons provides a wonderful opportunity to see a wide range of patients and to work with various specialists. I really appreciate the position I have been given to help patients with so many resources. I decided to write my blog post about traumatic brain injury patients because so many of them left an impact on my career and even my life. I wanted to take the chance to put the spotlight on TBIs in the optometry world! I look forward to continue to develop my career and education. Hopefully, I will even see some of you out on the hiking trails or kayaking in our beautiful local waters!