Many of us have experienced the frustration of doing all that is required to properly diagnose and treat an eye condition and having our treatment not work as well as we planned. You’re left wondering if you chose the wrong drug, the wrong dose, or maybe it was the incorrect diagnosis. Making things even more difficult is the very real chance that your patient isn’t properly adhering to their eye drop regimen.
As eye care professionals, we rely heavily on the assumption that our patients can and will instill drops in their eyes at the frequency in which we prescribe. Unfortunately, this is oftentimes an incorrect assumption. In order to better treat our patients’ eye conditions, it is important to remind ourselves of the barriers to good drop compliance and what techniques we can use to help overcome them.
Understanding Diagnosis and Treatment
The first step toward good drop regimen adherence is communication. Good communication starts in the exam room and includes explanation of both the diagnosis and the treatment. For symptomless diseases like glaucoma it can be difficult for patients to be motivated to obtain drops and learn how to instill them, let alone remember a sometimes-complex drop regimen. If the patient understands what disease they are treating and how not treating may impact their life, they will be more inclined to deal with the inconvenience.
Cost
After you did all you could to make sure the patient understands the what and why of their treatment, you send the drop prescription to the pharmacy, where the patient will find another hurdle – cost. The cost of eye drops can be prohibitive, especially new medications on the market that don’t have a generic alternative. The patient is often left with the choice of eating the cost or calling back to request an alternative. To help overcome this barrier, try prescribing generic medications whenever possible. It may be necessary to fill out a prior authorization to get the patient’s insurance plan to cover a branded medication.
Difficult to Administer
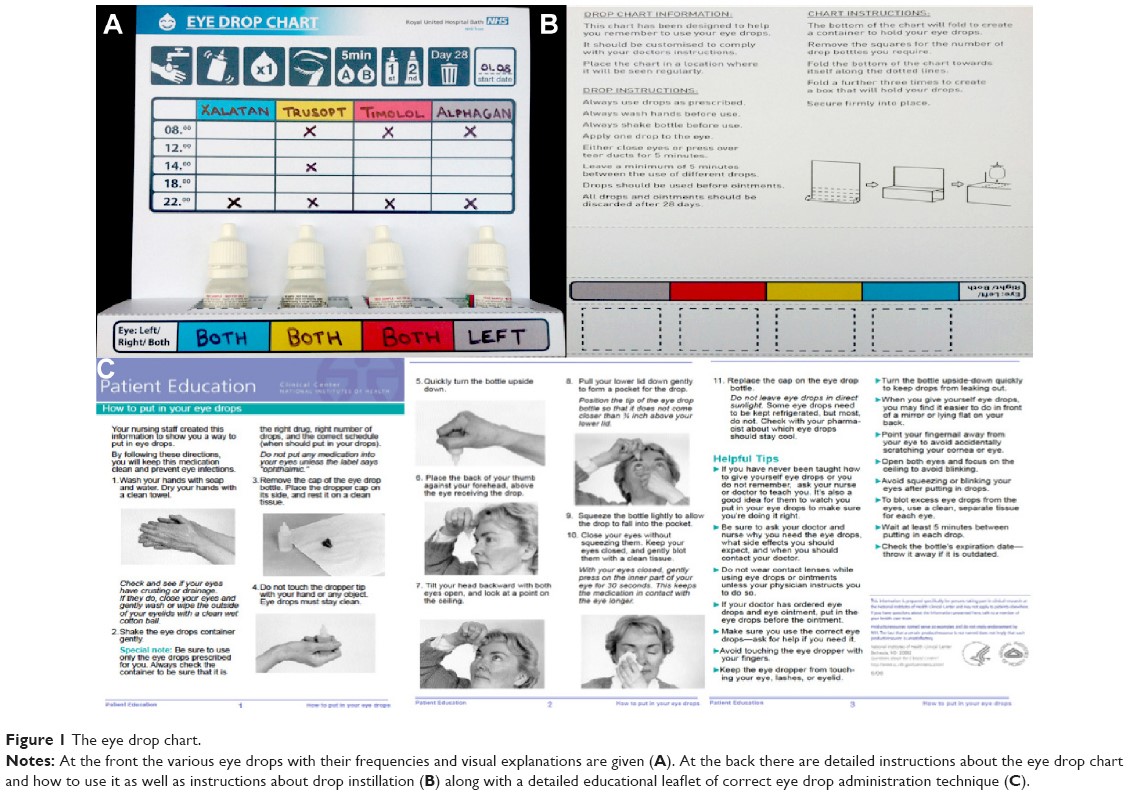
Effectively instilling drops is not a skill most patients are born with. The small bottles are difficult to squeeze, it’s difficult to accurately aim the drop into the eye, and putting anything in to the eye comes with a great deal of anxiety for many patients. It is helpful to discuss and even act out drop-instillation techniques with the patient before prescribing. Another option you have is to provide literature that describes proper technique, such as the eye drop chart, pictured below.1
Once the patient successfully instills the drop, it may cause stinging, itching, redness, or pain. If you discuss and plan for these side effects ahead of time, the patient may stick with the regimen more effectively. For example, warning patients that dorzolamide has a tendency to sting upon instillation or that brimonidine has a higher potential for allergic reaction and that the patient should discontinue the drop and call the clinic if allergic conjunctivitis symptoms occur.
Mental Hurdle
Having a drop regimen is not convenient and it can be difficult for patients to remember to instill their drops on time. Our older patients many times already have a long list of medications they are responsible for and adding a regimen of drops that can be upwards of 10 drops/day can be difficult, to say the least. For our younger patients, busy lifestyles with work and other engagements make it difficult to instill drops throughout the day. To help with this, you can provide for your patients written-out drop schedules, much like the one pictured above. Modern technology can also help patients remember to take their drops. You can recommend that your patients set alarms on their phones or download apps (such as NudgeCoach or MediSafe) that can regularly send notifications to your patients when it is time to take their drops.

Transparency
Many patients are uncomfortable with admitting to their eye care provider that they are having difficulty affording, administering, or remembering to take their eye drops. Unfortunately, this is still true for many patients, even when asked directly.2 As before, better communication can help. Having frank discussions with patients about the importance of compliance to their eye health can help patients see the benefits of discussing difficulties they may be having with their eye drops.
- McVeigh KA, Vakros G. The eye drop chart: a pilot study for improving administration of and compliance with topical treatments in glaucoma patients. Clinical ophthalmology (Auckland, NZ). 2015;9:813.
- Winfield AJ, Jessiman D, Williams A, Esakowitz L. A study of the causes of non-compliance by patients prescribed eyedrops. British Journal of Ophthalmology. 1990 Aug 1;74(8):477-80.

Author: Joshua Clermont, OD
Seattle clinic
I selected this topic because patient drop compliance is one of the biggest challenges that we as eye care professionals have when treating eye disease. My specific interest in eye care is glaucoma, where drops are the primary treatment and therefore present a daily challenge for my patients. I like working at Northwest Eye Surgeons because it allows me to focus on what I love most about eye care, treating ocular disease.









