XEN gel stent (Allergan PLC, Irvine, CA, USA) has recently made an exciting breakthrough into the minimally invasive glaucoma surgery (MIGS) market and is proving to be a reliable surgical option. Our Seattle glaucoma team at Northwest Eye Surgeons considers XEN stent to be an excellent alternative to the more traditional trabeculectomy at lowering ocular pressure and reducing patient need for topical therapy. This blog post will help explain its worthwhile advantages for the patient, surgeon, and glaucoma care provider.
What is XEN?
XEN gel stent is an FDA approved device developed by Dr. Rohit Varma which allows passage of aqueous humor from the anterior chamber to the subconjunctival space.1 The stent, about the length and width of an eyelash, is made from a hydrophilic collagen-based gelatin material which allows it to be biocompatible and highly flexible once inserted. Preloaded in a disposable XEN injector, the device can be placed in an ab interno fashion by means of a self sealing clear corneal incision or now via an ab externo fashion where it is inserted through a small transconjunctival incision.
Gaining FDA approval in November 2016, XEN45 gel stent was indicated for patients with refractory glaucoma who have failed on other types of surgical management and in patients with uncontrolled POAG, pseudoexfoliative glaucoma, or pigmentary glaucoma on maximally tolerated medical treatment. The XEN stent is categorized as a MIGS procedure since it circumvents the conjunctival dissection utilized in surgeries requiring a scleral flap and is currently the only MIGS that permits subconjunctival filtration.2
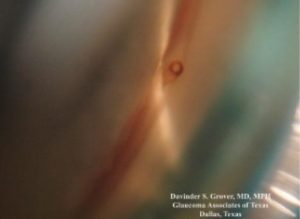
Figure 1. XEN45 gel stent as viewed by gonioscopy. Photo courtesy of Dr. Davinder Grover
Effectiveness.
The first studies of XEN45 gel stent showed promising results with IOP reduction and less need for hypotensive eye drops postoperatively. Pérez-Torregrosa et al3 demonstrated a 29.34% reduction in IOP at twelve months with a 94.57% decrease in medication. De Gregorio et al4 supported effectiveness with 41.82% reduction of IOP with 80.4% of patients off medication at twelve months.
Due to XEN’s recent arrival to the glaucoma market, prospective studies are currently underway to compare head to head success of XEN stent with trabeculectomy. A small retroactive analysis conducted by Dr. Ramesh Ayyala concluded that at one year follow up, mean IOP was significantly lower with trabeculectomy versus XEN stent implant.5 Overall success, however, at meeting therapeutic target was reasonably equal with the XEN group if adjunctive topical hypotensive therapy was added. Another earlier retrospective study within an academic setting demonstrated that there was no difference in efficacy, risk of failure, or safety profile between the two procedures.6 It is also widely accepted that restricted flow through the XEN stent creates less risk of postoperative hypotony when compared to more invasive glaucoma surgery.2
Postoperative Management.
Our goals with glaucoma surgery at Northwest Eye Surgeons include controlled and predictable ocular pressure along with fewer postoperative complications. When achieved these facilitate a reduction in the number of postoperative visits. MIGS are considered less surgically invasive by causing less tissue disruption and offer quicker healing time for our patients. Both the amount and course of postoperative anti-inflammatories can be reduced when compared to glaucoma surgeries requiring scleral flaps. MIGS procedures are also sutureless thereby eliminating appointment time required for suture removal.
Similar to trabeculectomy, XEN stent surgery is only successful if a conjunctival bleb is created perioperatively and carefully maintained postoperatively. Anti-scarring agents such as Mitomycin C and fluorouracil (5FU) are utilized during and following the procedure to counteract conjunctival scarring which threatens proper filtration. Encapsulation of the XEN bleb is a complication that needs an immediate diagnosis so that proper bleb management efforts can be employed. In a multicenter prospective study conducted by Grover the postoperative complication most reported was conjunctival bleb scarring requiring needling.7 Careful gonioscopy can also ensure that the XEN stent is properly placed as the device can occasionally become kinked or obstructed by iris anatomy.

Figure 2. XEN45 gel implant at 6 months with proper, low overlying bleb. Photo courtesy of A De Gregorio et al.2
Future of XEN.
Minimally invasive glaucoma surgery remains without a doubt a hot topic in glaucoma research. It goes without saying that despite all of MIGS advantages there still remains a need for traditional trabeculectomy and tube surgery. XEN stent has risen as but one great option amongst a large arsenal of modern day glaucoma surgeries. As no surgery in glaucoma is foolproof, we can only adapt to a shifting culture of care and employ alternative surgical management if our first attempt proves unsuccessful. It seems safe to say that in today’s healthcare setting, the effective but less invasive surgical strategies requiring fewer postoperative visits will continue to drive the evolution of XEN stent and its fellow MIGS procedures.
- Snelling S., November 2016. Breakthrough refractory glaucoma treatment cleared by FDA after clinical trials. Keck School of Medicine of University of Southern California, https://keck.usc.edu/breakthrough-refractory-glaucoma-treatment-cleared-by-fda-after-clinical-trials/ (August 4, 2019)
- De Gregorio A, Pedrotti E, Stevan G, et al. XEN glaucoma treatment system in the management of refractory glaucomas: a short review on trial data and potential role in clinical practice Clin Ophthalmol. 2018; 12: 773–782.
- Pérez-Torregrosa VT, Olate-Pérez Á, Cerdà-Ibáñez M, et al. Combined phacoemulsification and XEN45 surgery from a temporal approach and 2 incisions. Arch Soc Esp Oftalmol. 2016;91(9):415–421.Spanish.
- De Gregorio A, Pedrotti E, Russo L, Morselli M. Minimally invasive combined glaucoma and cataract surgery: clinical results of the smallest Ab interno gel stent. Int Ophtalmol. 2017 May 29; Epub.
- Salim S, Ayyala R., May 2019. Xen vs. trabeculectomy: a retrospective analysis. American Academy of Ophthalmology, The Ophthalmic News and Education Network, https://www.aao.org/interview/xen-vs-trabeculectomy-retrospective-analysis (August 4, 2019)
- Schlenker MB, Gulamhusein H, Conrad-Hengerer I, et al. Efficacy, safety, and risk factors for failure of standalone Ab interno gelatin microstent implantation versus standalone trabeculectomy. Ophthalmology. 2017;124(11):1579–1588.
- Grover DS, Flynn WJ, Bashford KP, et al. Performance and safety of a new Ab interno gelatin stent in refractory glaucoma at 12 months. Am J Ophthalmol. 2017;183:25–36.
 Author: Landon Jones OD FAAO
Author: Landon Jones OD FAAO
Seattle clinic
I am honored to be part of the Glaucoma & Cataract MD-OD Partnership team at Northwest Eye Surgeons with Drs. Bruce Cameron and Josh Clermont. In this model of practice I can be a more prominent stakeholder in both the surgical plan and the ongoing treatment plan postoperatively. I have also enjoyed collaborating with fellow optometric colleagues as glaucoma becomes more and more common in the primary eye care setting.









